This article was published in March 2020 and may not reflect the latest scientific research on COVID-19 vaccines. We encourage you to stay up-to-date on COVID-19 news from your local health authority.
Science World is actively taking measures to enhance the health and safety of our guests, which are and continue to be our priority. Learn what we're doing to implement appropriate precaution within our facility.
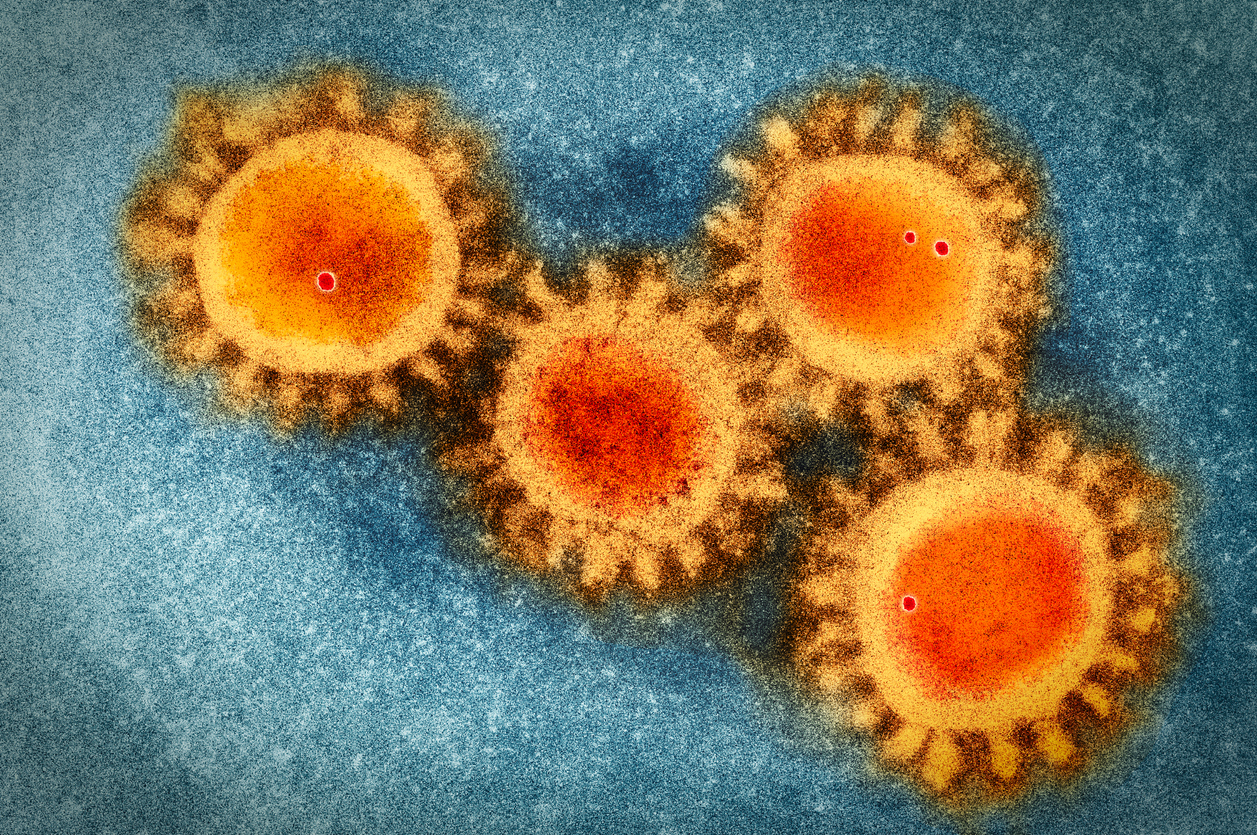
Coronaviruses are a large family of viruses found in animals, with a few cases found in humans causing respiratory illnesses like the common cold. Previous outbreaks have led to diseases such as SARS (severe acute respiratory syndrome), which was eliminated from the human population through a global effort in 2003.
The novel coronavirus is causing a disease known as COVID-19, which appears to have a mortality rate lower than previous outbreaks of MERS-CoV and SARS-CoV. We spoke to Dr. Eleni Galanis of the BCCDC to get a better sense of what actually happens when you get the coronavirus, what we can do and some of the common misconceptions about this outbreak.
What makes COVID-19 different to previous coronavirus-related diseases like SARS and MERS-CoV?
The new coronavirus is called SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) because it is closely related—but not identical—genetically to the SARS-CoV. The disease it causes is called coronavirus disease (COVID-19) which includes a mild respiratory illness like the common cold. However, it can also cause severe illness in a subset of people such as the very old, frail or immunocompromised.
What is the risk of the coronavirus to those who are not immuno-compromised?
People who may be at risk of being exposed to the #coronavirus are those who have been in close proximity to someone who is infected. #Covid19 pic.twitter.com/fl67s2UawJ
— BCCDC (@CDCofBC) March 3, 2020
Because the symptoms of the Coronavirus are similar to cold and influenza, how do healthcare workers properly determine someone has COVID-19?
It is difficult to differentiate the COVID-19 virus based on symptoms alone. Because currently it is not yet well established in the human population, especially in Canada, health care workers ask about patients’ travel history to help them identify COVID-19 as a possible cause of respiratory illness. If a patient has travelled abroad to regions affected by COVID-19, this will increase the level of suspicion for it.
Also, health care workers can test patients to differentiate between viruses. A COVID-19 (SARS-CoV-2) test exists in BC to help diagnose this infection.
How are facemasks and sanitizer helpful or unhelpful?
One point we should consider is that people who wear face masks may be more likely to touch their face, thereby increasing the risk of infection. For prevention, regular face masks (also known as surgical masks) can protect the nose and mouth against infection spread by droplets. Droplets are larger than the pores in the mask, and the mask acts as a barrier, protecting the mouth and nose. If masks are not worn properly or get wet, they may be less effective. In addition, masks do not protect the eyes.
Frequent handwashing with soap and water for 20 seconds is an effective way to prevent the spread of infection. But if water is unavailable and hands are not visibly soiled, hand sanitizer containing at least 60% alcohol is also effective at eliminating viruses.
What’s entailed in developing a vaccine for the novel coronavirus?
In general, safe and effective vaccines are the best line of defence against infectious diseases. Unlike influenza, there is currently no vaccine against COVID-19, but the search for vaccine candidates is already underway globally. We may learn of some promising options in the coming months.
It can take a decade for a new vaccine to be proven safe and effective for broad use in the population, although with concerted global effort, this process may be expedited.
Vaccine discovery and development for population use follow particular protocols:
- The first step is laboratory work to identify the antigen or virus particles that will be used in the vaccine.
- The next step is a series of animal studies to assess the safety of the vaccine and its ability to generate an immune response.
- Then, three phases of human vaccine trials are required:
- Phase 1 is conducted on a small number of people to assess the safety of the vaccine and the type of immune response it provokes.
- Phase 2 is conducted on a larger group of people, including a subset which receives a placebo, to assess safety, immunogenicity, dosing, schedule and method of delivery.
- Phase 3 is a randomized study conducted with tens of thousands of people where the vaccine is compared to a placebo and safety and efficacy is measured.
Is there a good checklist for when we should be washing our hands?
Wash hands with soap and water:
- before leaving home and on arrival at another location
- after using the toilet
- before food preparation
- before eating any food
- after having touched other people or surfaces
Want to keep up-to-date on the novel coronavirus?
The BCCDC has developed a resource page (available in multiple languages) to answer frequently asked questions about the virus including its risk assessment and how BC is preparing for the spread of COVID-19. You can also check the Government of Canada's outbreak update page for more information.